Home Semen Analysis Kit
If you are concerned about your fertility, the first test
you need to do is to get your husband to agree to get his semen tested.
Now, this can be embarrassing – after all, it’s no fun being
forced to produce a semen sample on demand in the dirty bathroom of a clinical
lab ! Also, he is secretly petrified that he may be shooting blanks, which is why
he is very reluctant to get the test done. His worry is that a poor result will
cast aspersions on his masculinity, and this is why the ability to do your own
semen analysis at home can be such a blessing. Yes, a semen analysis report
from a reliable pathology lab is still the gold standard, but there’s a lot of
valuable information a Home Semen Analysis can give you.
And while it’s true that any pathology lab can readily check
a man's sperm sample, the problem is these reports are highly unreliable. The
lab tech is often untrained, and they fill in the results without checking or
verifying them. Unreliable lab results can fool you – and this can be an
expensive error.
The best solution to do your semen analysis for
yourself, which allows you to observe
and count your sperm on your own. The good news is you don’t need to be a
scientist or a biology buff to be able to do this. We have made this very easy
for you !
What is included
in the Home Semen Analysis Kit?
- Mini-microscope -To check your sperms
- Clamp, to attach your smart phone to the eye-piece of the
microscope
- Semen container
- used to collect semen samples
- Glass Examination
Slides - To examine your sperm under a microscope. You used these in your
high school biology classes, remember ?
- Prestained Slide
( CryoLab) - To verify your Sperm count. The Prestained Slide contains chemical
on the surface which will make the sperms immotile and make it easier to count
the sperms (Total Sperm count)
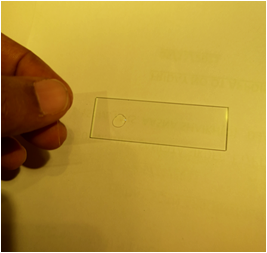
- Dummy Examination Slide - This dummy slide will aid in
focusing the microscope
- Cover Slips - These are thin baby slides, and are used to keep
the semen sample from drying out. You will need to cover the semen drop with a
cover slip when analyzing this
- Pasteur pipettes
to handle your semen sample.
Analyze your semen
sample step by step -
1) Collect your semen sample in the container provided. This
is single use, sterile and disposable.
2) Clean the Examination glass Slide with the Alcohol Swab
to remove the dust on the slide. You can alternatively use Hand Sanitizer. Put 2-3 drops of sanitizer on the glass slide and clean it with tissue paper

3) Now Open the sterile Pasteur pipette by unpeeling the
package, and use it to mix the sperm sample well.
Use the pipette to suck up the sample and deposit a single drop
on the glass slide. The size of the drop is not critical because the sample
will spread on its own
Also, add a drop of the semen on the CryoLab slide and keep
this on the side for now.
4) Place a cover slip over the drop (both on Examination
slide and CryoLab Slide) to prevent the sample from evaporating.
5) Turn the Focus Ring all the way to the right.
6) Attach the microscope clamp to the camera lens of your
mobile phone.
7) Finally, secure the clamp in the eyepiece slot of the
microscope.
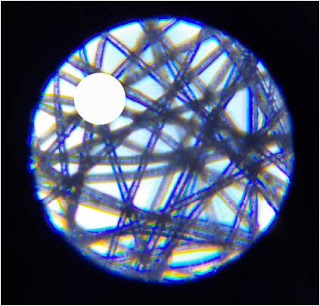
8) Place the Dummy Slide in the slot beneath the microscope.
Move the Zoom to the extreme Left (100x Magnification).
Now slowly shift your focus Ring to the left until you see
the threads of the cloth on dummy slide clearly (as shown in the below image)
Move the zoom to Extreme right (250x)
9) Now without disturbing the Focus Ring, Place the Examination
glass slide with your Sperm sample in the slot beneath the microscope
10) You will see your Sperms clearly . If you are not able
to see the sperms slowly shift the focus to the left or right until the sperms
are clearly seen.
The Zoom will always need to be set to maximum (250x) to
identify sperm
You are now ready to start admiring your sperm !
So, what do sperm look like ?
There are 2 kinds of sperm – motile ( those which move) and immotile ( those which don’t).
It’s easy to identify moving sperm because they are moving,
but it can be hard to count them because some of them move so rapidly.
It’s easier to count immotile sperm, but it can be easy to
confuse them with other cells in the semen (such as pus cells) or dust on the slide,
and this can mislead you.
12) Increase the zoom on your phone camera to 2.5 times.
With zoom, you don't have to be precise. Anything close to
2.5x will suffice.
This will make it easier for you to count the sperms.
In the light field, count the number of moving (Motile)
sperms.
This can be hard to do because your eye gets attracted by
the motion, but don’t worry too much about accuracy for now.
You can take 2-3 measurements, and then calculate the
average if you want to be more precise. Do this as a joint exercise!
Make a note of this on a piece of paper
B = Motile Sperms
If you see 15 moving (motile) sperms in the light field
(2.5x zoom on camera), that suggests there are 15 million motile sperms in 1 mL
of your sperm sample.
This is approximate count !
A rough estimate.
We tried this using the Makler's Sperm Counting Chamber as a
reference and discovered that the number of sperms at 2.5x magnification is
quite similar to the actual count.
13) Take a picture with your Phone's camera (or Screenshot)
14) Make a note of the number of sperms in the screenshot
image.
A = Total Sperms
Total Sperms (A) = 30 sperms in this example (That means
there are Total 30 million sperms in 1 ml of Semen Sample)
The number of sperm in your sperm sample = A (millions)
(B/A * 100) percent Motility
Motility = 15/30*100 = 50% in this example.
How do you verify your results ? This is where the
pre-stained slide comes in
Place a drop of your Semen using a Pasteur Pipette on the Stained
Part of the pre-stained slide (Dark Red part on the slide)
Leave this for 30 min. The Chemical on the Slide will make
the Sperms immotile.
Now keep the slide under the microscope and take a
screenshot.
This will allow you to count the No. of Sperms, all of which
will be immotile, so counting them will be easier. You can cross-check this
number with the total sperm count which you made a note of in Point No. (14)
How do you
interpret the sperm count and motility?
The Sperm Count measures the number of sperm in 1ml of your
Semen Sample
Don’t panic if you can’t see anything ! You may be nervous
and not be able to focus the lens properly. Try doing the test again in 2 days.
If you still can't see any sperms, it means you're
sperm count is NIL. The Medical Terminology for this condition is Azoospermia.
You should see a urologist, who will examine you and
determine the cause of your lack of sperm. Sperm absence is most commonly
caused by an obstruction in the reproductive tract.
2) Sperm Count: 0 to 15 Million Sperm = Sperm Count is Low
3) A good sperm count is more than 15 million sperms.
Frequently Asked
Questions:
1) Who can benefit from a home sperm analysis?
Ans a) For men
who wish to start a family but are concerned about their sperm count
b)For
those who do not want to go to a pathology lab to have their semen sample
checked for a variety of
reasons, such as being embarrassed to generate a semen sample in a pathology
lab or having mistrust in pathology labs.
c) For
those who have had a Vasectomy and wish to be certain that their Sperm Count
has dropped to zero.
d) For
people who are using sperm count-increasing drugs and wish to keep track of how
much their sperm count is
increasing.
2) Is it simple to use the Home Semen Analysis Kit?
Ans The Home
Semen Analysis kit is simple to use provided you follow the instructions.
3) What is the appearance of sperm? How do we tell the
difference between sperm and other things?
Ans A sperm has
two parts: a head and a tail. The tail is what distinguishes sperm from
other cells found in the sperm
4) What should we do if there are too many motile sperms to
count?
Ans You have
nothing to be concerned about. It means that your sperm sample is exceptional
in terms of quality.
Troubleshooting
and Problems
1) If you're having trouble concentrating and seeing the
sperms, turn the focus Ring all the way to the right and slowly move it to the
left until you see sperms.
2) You haven't clamped the phone camera on the eyepiece if
you can't see anything in the phone.
Fixing the mobile camera lens in the clamp and then the
clamp in the eyepiece slot is the proper procedure.
Home semen analysis
has some drawbacks.
1) While
we can get a rough idea of sperm count and motility using a home semen analysis
kit, this is not as reliable as a semen analysis done in a well-equipped
pathology lab by an experienced technician. This is still the gold standard.
2) Also,
we can't check the morphology (sperm shape ) with a home semen analysis kit. To
examine the morphology of sperms, a considerably higher magnification is
required, which our mini-microscope lacks.
Please
email us at  ivflab@drmalpani.com have any questions or require
assistance with the home semen analysis kit.
ivflab@drmalpani.com have any questions or require
assistance with the home semen analysis kit.